Are Peptide-Drug Conjugates the Future of Oncology?
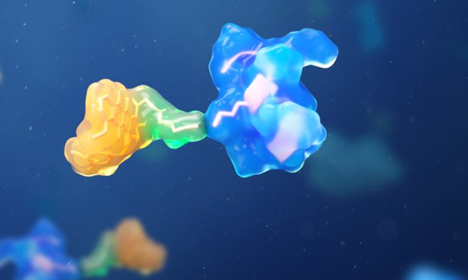
Peptide-drug conjugates (PDCs) represent a promising development in cancer therapeutics, offering a strategic approach to delivering drugs directly to tumor cells. By coupling peptides with potent anti-cancer agents, PDCs aim to enhance the precision and efficacy of treatment. These conjugates leverage the selectivity of peptides for specific targets, minimizing the impact on healthy cells. With cancer being a major cause of mortality worldwide, the innovation presented by PDCs could transform treatment paradigms. Scientists and researchers are now exploring this novel technology to overcome the limitations of traditional therapies. This blog delves into the advantages, innovations, challenges, and future outlook of PDCs in the field of oncology.
Advantages of PDCs Over Traditional Therapies
Peptide-drug conjugates (PDCs) present several notable advantages over traditional cancer treatments, addressing some of their inherent limitations. One key benefit is their ability to selectively target tumor cells, which helps reduce off-target effects. This specificity can lead to improved patient outcomes. Additionally, PDCs can deliver higher concentrations of drugs directly to cancer cells, enhancing therapeutic efficacy. By reducing systemic toxicity, these conjugates minimize the adverse side effects often associated with conventional chemotherapy. As a result, PDCs have the potential to offer patients a more effective and tolerable treatment option.
Enhanced Tumor Penetration and Selectivity
The enhanced tumor penetration and selectivity of peptide-drug conjugate are major factors driving their appeal in cancer therapy. By utilizing peptides, these conjugates are engineered to recognize and bind specific receptors on tumor cells with high affinity. This precise targeting increases the concentration of cytotoxic agents directly at the tumor site, bypassing healthy tissues. Consequently, PDCs improve the therapeutic index and limit collateral damage to normal cells. Additionally, peptides can penetrate deeper into tumor masses, overcoming the traditional barriers that limit drug delivery. This increased intratumoral concentration of the drug enhances its ability to exert cytotoxic effects effectively, paving the way for more successful treatment outcomes. As ongoing research unfolds, the potential for PDCs to address currently untreatable tumors is expanding, marking a significant advancement in cancer care.
Reduced Immunogenicity and Manufacturing Costs
PDCs also offer the advantage of reduced immunogenicity compared to antibody-drug conjugates. Peptides, by their nature, are less likely to provoke an immune response due to their smaller size and structural simplicity. This attribute diminishes the risk of adverse immune reactions, making treatment more predictable and safe. Additionally, the manufacturing of peptide-drug conjugates tends to be more cost-effective than that of traditional biologics. Peptides can be synthesized chemically, enabling more straightforward production processes and scalable manufacturing. This can lead to lower production costs and expanded access to novel therapies. Moreover, the stability of peptide-based conjugates during storage and transportation further adds to their economic advantages. Reduced immunogenicity combined with cost-effective manufacturing positions PDCs as a viable and attractive option in oncological treatment designs.

Improved Pharmacokinetics and Biodistribution
Improved pharmacokinetics and biodistribution are pivotal benefits of peptide-drug conjugates (PDCs) in cancer treatment. The conjugation of drugs to peptides facilitates their absorption, distribution, metabolism, and excretion properties, optimizing therapeutic potential. Peptides can be designed to resist proteolytic degradation, improving drug stability in the bloodstream and extending half-life. This prolongs the drug’s presence at the tumor site, enhancing its therapeutic impact. Moreover, PDCs can be engineered to adjust biodistribution patterns, directing the drug to specific tissues or cells while avoiding non-target areas. This selective delivery fosters a more potent and localized therapeutic action, mitigating systemic side effects. Researchers are leveraging these properties to create more precise and personalized cancer treatments. Enhanced pharmacokinetics and biodistribution are, therefore, crucial attributes that strengthen the case for PDCs as a transformative approach in oncology.
Innovations in PDCs Design and Delivery
Recent advancements in PDCs design and delivery systems have pushed the boundaries of cancer treatment. Innovative strategies include optimizing linker technologies that connect the peptide to the drug, enhancing stability and controlled release. These advancements ensure that drugs are released at appropriate therapeutic doses only upon reaching the target site, bolstering efficacy and safety. Researchers are also exploring novel targeting moieties beyond traditional receptor targeting to include tumor microenvironment-responsive elements. Such elements help in the selective activation of the drug in the cancerous milieu. Additionally, integrating modern delivery systems like nanoparticles improves penetration and retention within tumors. These innovations are progressively refining PDCs, shaping them into adaptable and effective therapeutic tools in the oncology landscape.
Challenges in PDCs Development
While PDCs hold remarkable promise, their development is not without challenges. One significant obstacle is ensuring the stability of the conjugate in systemic circulation to avoid premature drug release. This requires meticulous design of the peptide linkers to withstand biological conditions. Additionally, achieving optimal in vivo selectivity and avoiding non-specific tissue uptake remains complex. There are concerns about the cost and time-intensive nature of clinical trials required to confirm safety and efficacy. Moreover, the heterogeneous nature of tumors poses difficulties in creating universally effective PDCs across diverse cancer types. Addressing these challenges calls for concerted research efforts and innovative technological approaches.
Future Perspectives in Oncology
The potential of PDCs in oncology signifies a transformative shift towards precision medicine. As research progresses, we anticipate their integration into personalized treatment regimens, significantly improving cancer management strategies. Exciting possibilities include synergistic combinations with other therapies to overcome resistance mechanisms and enhance treatment outcomes. Further advancements in biomarker identification will likely streamline patient selection and optimize therapeutic response. Additionally, broadening the application of PDCs beyond oncology to other therapeutic areas could revolutionize treatment paradigms in chronic diseases. The future of PDCs in oncology thus holds immense potential, underscoring their role as pivotal contributors to next-generation medical solutions.
Conclusion
Peptide-drug conjugates are reshaping the future of cancer treatment, highlighting a new era of targeted therapy. By maximizing drug delivery to tumors while minimizing side effects, PDCs hold the potential to enhance patient outcomes significantly. Although challenges exist, ongoing research and innovation continue to break barriers and harness the full capabilities of this technology. As scientific advancements progress, peptide-drug conjugates are anticipated to become integral to personalized cancer therapies, representing a leap forward in precision medicine. These developments mark a promising time for oncology, offering hope for more effective, accessible cancer treatment options.







